Background: Tixagevimab-Cilgavimab (Evusheld or AZD7442) is a combination of two monoclonal antibodies directed against viral spike proteins from binding to hosts' enzyme receptors, thus blocking viral entry into cells. The drug is FDA approved for use as pre-exposure prophylaxis (PrEP) in immunocompromised patients including Allogeneic hematopoietic stem cell transplant (Allo-HSCT) recipients. It has potential to both prevent and treat COVID-19, reducing incidence of severe infections and death for up to 6 months. Allo-HSCT patients are at higher risk of COVID-19, and may fail to mount a robust immune response to vaccination. In this study, we investigate the efficacy and safety of Evusheld in Allo-HSCT recipients 6 months following transplant at our institution.
Methods: We performed a retrospective analysis of Allo-HSCT recipients treated at our institution between January 2021 to January 2023. Descriptive statistics related to the participant baseline characteristics, treatment, and transplant data were reported. The incidence of COVID-19 infections and safety data between two groups (Evusheld versus non-Evusheld) were estimated.
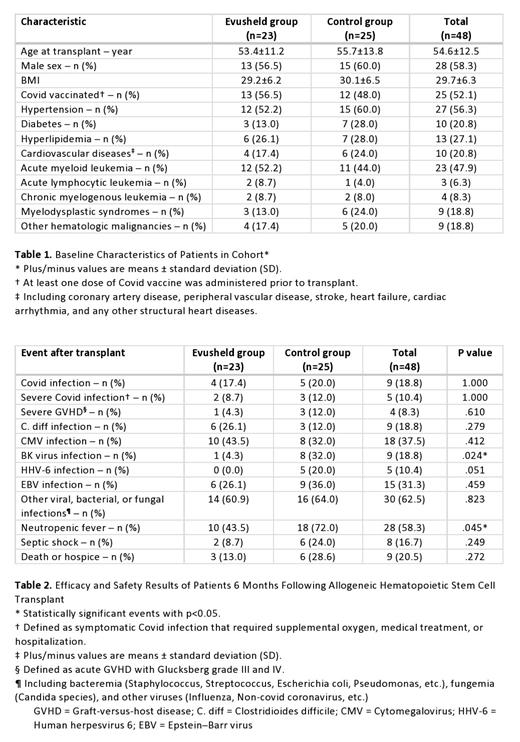
Results: A total of 48 Allo-HSCT recipients were included in our study, 23 (47.9%) patients received PrEP Evusheld. The median age at transplant was 54.6 years. Patients were predominantly males (58.3%). Notable comorbidities included hypertension (56.3%), diabetes (20.8%), hyperlipidemia (27.1%), and cardiovascular diseases (20.8%). Indications for transplant included acute myeloid leukemia (47.9%), acute lymphocytic leukemia (6.3%), chronic myelogenous leukemia (8.3%), myelodysplastic syndromes (18.8%), and other hematologic malignancies (18.8%) (Table 1).
The efficacy and safety results of Evusheld were shown in Table 2. The median time from transplant to Evusheld administration was approximately 100 days. There was no significant difference in the incidence of Covid infection (RR=0.842, 95% CI: 0.196-3.615, p=1.00) or severe Covid infection (RR=0.69, 95% CI: 0.10-4.60, p=1.00) between the two groups following transplant. All-cause mortality (death or hospice) was also comparable between the two groups (RR=0.375, 95% CI: 0.080-1.748, p=0.272).
The rate of severe acute graft-versus-host (GVHD) and infections were comparable between the two groups, including clostridium difficile, cytomegalovirus (CMV), BK virus, human herpesvirus-6 (HHV-6), Epstein-Barr virus (EBV), and other bacterial and fungal infections.
Conclusions: Our study found no evidence of efficacy of Evusheld against COVID-19 after Allo-HSCT transplant. This lack of efficacy may be attributed to the emergence of the XBB.1.5 subvariant of omicron during the study period. We also found no difference in all-cause mortality between the two groups. Further data is required to gain a comprehensive understanding of the potential use of Evusheld in transplant populations.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal